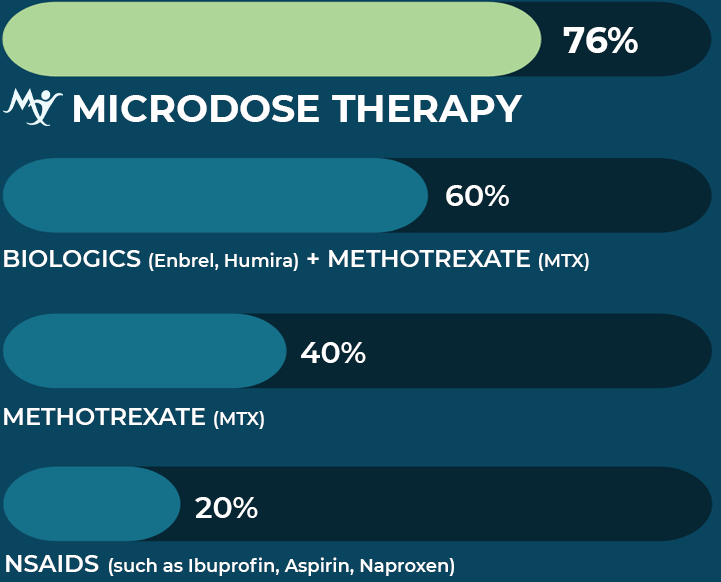
Cortisol is the only body-made substance capable of extinguishing the out-of-control inflammation within inflammatory and autoimmune diseases. Since only the patient knows when natural, beneficial inflammation like from an injury is going out of control by experiencing increasing pain and related symptoms, it is the patient who must take cortisol tablets only at this time of bad days and not during good days. Used in this way and having been taught the safe use limit of cortisol, patients do not exceed the safe use limit and superior pain and related symptom control is achieved. The patient gains control of the disease, not the disease over the patient.
LOSE MOST PAIN IN 3 WEEKS
Your response to cortisol will be rapid. For the first three weeks, you will be taking cortisol tablets daily to extinguish your pain and related symptoms. Then, we will teach you how to take smaller regimens of cortisol to extinguish reoccurring flares. In doing so, you will consume less cortisol than the safe daily use limit of cortisol.
To use Microdose TherapyTM, you must be trained when, how much, and for what reasons to use cortisol tablets. The Helen Foundation tele doctor will prescribe your cortisol tablets and help you use it via telemedicine, our Microdose TherapyTM Patient Education Manual, and the electronic daily monitor with guidance by a Helen Foundation coach.